CB is 4 years old …
I touched on CB’s diet in an earlier blog, but I don’t think I have gone through CB’s evaluation, therapy, and treatment history.
CB was 10 months old when his daycare provider informed us that CB was developmentally behind and did not seem to catch on to things like his peers. This was extremely hard to digest.
CB’s first introduction into the therapy world was with a warm, yet challenging Physical Therapist. He was 15 months old. She helped CB learn to walk. He started walking (ability to walk across a room) at 17.5 months. His PT would push him further than I ever would but she knew just how much to push him to help him grow and move past some of his frustration. It was a good experience and we ended therapy shortly thereafter.
CB started gymnastics at around 19 months old. We thought it pretty much worked kind of like PT as it got him moving and trying new and different physical activities. He hated the big parachute for most of the year and needed a lot of herding to keep him somewhat engaged.
The month after CB turned 2, he was evaluated by a PROMPT speech therapist and given the diagnosis of a moderate receptive-expressive language disorder and a moderate-severe neuro-motor speech disorder. He started PROMPT speech therapy the following week 1x a week. The next month, Early Childhood Intervention (ECI) evaluated CB and determined that he had a significant speech delay. They started their services within the month and came to our house 1x a week. The ECI interventionalist helped CB with speech and social skills (i.e., sharing, taking turns). After 3 months of private ST, it was determined that the PROMPT speech therapist, although nice, was not pushing CB enough. We decided to end private ST and continue with just ECI. About 2 months before CB turned 3, a licensed ST from ECI started coming to the house 1x a week, as well. CB progressed but at a pretty slow pace. ECI evaluated CB for OT help but he was not far enough behind to get help. Although, I think if I had replied more accurately, he would have qualified. As a parent new to the special needs processes, I responded to most things with the best case scenario response. I think I replied that he ate pretty well with a fork and spoon. He still doesn’t eat well with a fork and spoon. It is still challenging and he gets food all over himself 9 out of 10 times when eating. ECI was helpful in training us how to talk to CB and how to play in a more helpful manner. My husband and I are not huge talkers so it felt very unnatural to talk about what we were doing all the time and to repeat what CB was saying. I think this information helped us tremendously and helped CB’s confidence. When we started saying what we understood him to be saying and not phrasing it as a question, I think he started to feel that we really understood him.
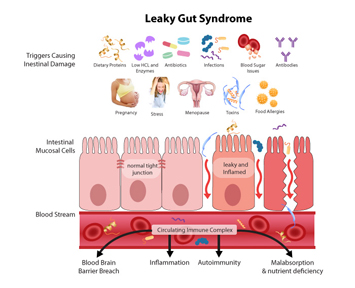
At 2 years 11 months, the school district evaluated CB and determined that he qualified for the PPCD (Public Preschool for Children with Disabilities) program due to his delayed speech. For his school district evaluation, he mainly produced 2-3 sounds for everything. Most of his responses were bah, buh, or duh. When the evaluator asked if we thought the evaluation was representative of his skills, we responded proudly that we thought he tested well because he had tried to answer every question with a response. He normally didn’t do that. He many times wouldn’t even provide a response when you asked him to say a specific word or to repeat after you. CB received 2 private ST 15 minute sessions and 1 group ST session at PPCD. CB also started private ST at the same time 1x a week. 2 months later, CB started taking Nordic Naturals Fish Oil, Probiotics, and a multivitamin. AT 3.25 years old, CB’s pediatrician approved blood work due to CB’s chronic loose stools (sometimes with undigested food bits) and developmental delays.
During the summer, there was no PPCD so CB attended a language camp for a month. Then he took a month long break from therapy because we were out of the state traveling. He still continued to progress during the break. When the fall semester started up, CB moved to swim classes since he could not move up in gymnastics since he was not potty trained. I am so thrilled the switch was made. He absolutely loves his swim class and the class is only 2-4 kids total each class. He also started private OT services 1x a week and increased private ST to 2x a week. CB also started karate. It is a class for kids with special needs. At 3.75 years old, I determined from the blood work performed earlier that year that CB had a much higher than average chance of being celiac. The next day, our household went (GFCF) gluten-free and casein-free. Within 2 months, we saw improvements globally for CB from speech to gross motor to fine motor to sensory awareness (he could feel temperature changes outside). Our household also went soy-free within 1.5 months of going GFCF b/c CB started to present with a soy allergy. His ST sessions at PPCD remained the same. In March, we added Physical Therapy to his schedule to focus on integrating his retained primitive reflexes. He has a long list of unintegrated primitive reflexes. She also works on other gross motor skills, as well. I perform the developmental exercises at home anywhere from 2-6x a week. For most of the exercises, I have to do them in passive mode. Surprisingly, CB handles his schedule quite well and enjoys all of the activities.
Some things we have learned along the way 1) the PPCD structure has been extremely helpful for improving CB’s executive function, focus, attention, independence, social skills, speech and potty-training skills. 2) CB has visual, auditory, gross motor planning and execution, fine motor planning and execution, coordination and balance, food sensitivities, speech, and sensory issues 3) to listen to CB and to work within his limits and abilities 4) stop/change therapy if it isn’t working 5) seek answers and ask questions 6) even though we have heard it over and over again, we are our child’s biggest advocates.
Positive Progress: 1) CB is now completely in underwear except for diapers at night. He has been wearing underwear at school since the beginning of Dec but continued to have accidents on a regular basis. We let CB direct when he was ready to start wearing underwear at home and that is working out well. He also decided this week that he doesn’t want to wear diapers during naptime. He still needs quite a few reminders so that he pees in the toilet, and not accidentally in his clothes or on the floor. He even had 3 days accident free. Yay!!
2) We arranged to meet with an expert in the dyspraxia field in the upcoming weeks! We also have talked with a director of a motor planning and coordination lab. We are feeling very positive this week and feel we are moving in the right direction.
3) We upped CB’s fish oil earlier this week. He is now taking Nordic Naturals Omega Complete liquid form .He was CRAZY for about 2-3 days. However, his articulation, fluency, and the amount of language he used improved. He also climbed a new type of monkey bar about 6 -6.5 feet tall (4-5 times) to get on a playscape. It seems like in the past, the days/weeks or so following an increase in fish oil, CB makes a big jump cognitively, physically, and verbally. We then see a little dip and then a leveling off at a higher level from where CB started.
Low: CB still has light shiners under his eyes, a rash on his bottom, and some digestive issues periodically. Arghh…we have made quite a few diet changes but we still need to keep tweaking and testing to see what is still ailing CB.